Therapy procedures in the project
The project has two therapeutic focuses: arm rehabilitation and neurovisual rehabilitation for neglect.
Treatment modalities for arm rehabilitation used in the project are the arm ability training (AAT), the arm basis training (ABT), and mirror therapy.
Arm paresis is a major contributor to stroke-related disabilities of daily living. Together, the AFT and ABT represent a modular treatment concept (impairment-oriented training, IOT) with two systematic standardized forms of therapy with good and superior effectiveness to other forms of treatment (Platz et al., 2001; 2005; 2009; 2018).
Arm ability training
The arm ability training, developed by Professor Platz, is a specific treatment for patients with mild or moderate arm paresis. It can be used to train different independent specific sensorimotor functions with reduced capacity, e.g. the ability to perform rapid alternating movements with the fingers, the ability to keep the arm and hand steady, dexterity with the manipulation of objects and to perform aimed movements with the arm precisely. All these abilities are frequently impaired after acquired brain damage or other diseases of the nervous system. Affected persons notice this by the fact that the arm no longer can be used as dexterously, as quickly or as easily in everyday life. The arm ability training aims to increase the performance in all these different areas. It is not sufficient to train single abilities. Instead, all described abilities need to be trained systematically to improve the everyday competence of the affected arm.
Arm Basis Training
Severe arm paresis after stroke leads primarily to the inability to perform selective arm movements as the main focus arm dysfunction. I.e., in case of severe paresis individual muscles can either no longer be activated at all, or they can no longer be activated individually or specifically. Therapeutic goal in that situation is to reactivate innervation for all muscles group in the arm in such way that they can be controlled individually and in a selective way.
The arm basis training, developed by the physiotherapist Christel Eickhof, systematically and repetitively trains movements in all segments of arm and hand.
The arm can only be used optimally in daily life, if selective active movements in all segments of the arm and hand (e.g. shoulder joint movements, elbow joint movements, wrist joint movements, finger movements) have been restored.
Mirror therapy
The therapies described above, are complemented by the mirror therapy. Mirror therapy has been proven to promote functional recovery in everyday life, especially in cases of severe arm paresis (Thieme et al., 2018) and can be implemented without an assistant.
Mirror therapy aims to help the affected side of the brain, which is the one opposite the paretic arm, to re-gain control over it again. For this purpose, this half of the brain can be stimulated.
The brain is not only stimulated through movements themselves, but also through seeing the arm being moved. Seeing the arm movement reinforces the movement control of the brain.
Unfortunately, affected persons with severe arm paresis can no longer move their severely paretic arm, and hence no movement of the paretic arm can be perceived by the brain.
With a mirror, however, an illusion can be created. If the healthy arm moves and the affected person looks into mirror while doing so, he/she sees a mirror image that looks exactly like the other, paretic arm. While the healthy arm moves and the affected person looks into the mirror, he/she sees that the paretic arm appears to move quite normally. This apparently normal movement of the paretic arm in the mirror can then stimulate the affected half of the brain and thereby promotes its control for the affected arm.
Neurovisual rehabilitation (for neglect)
Neglect is a multimodal dysfunction of the spatial allocation of attention. The associated visual neglect of object, body, and space halves can cause a significant disability in daily life (Kerkhoff et al. 2018).
Standardized training methods for the treatment of neglect include the optokinetic stimulation with active gaze sequence movements (OKS), visual saccades or eye movement training to single stimuli, and visual exploration training with larger templates.
Optokinetic Stimulation:
In optokinetic stimulation therapy, dots or symbols on the screen move uniformly all together in one direction, towards the neglected half of the visual field. The patient is asked to fix his eyes on a symbol and to let the "cloud of dots" "pull" his view all the way to the edge of the screen and to remain there. In doing so, the brain of people affected by neglect can relearn to turn the gaze so far to the left (or right) as it can hardly do spontaneously.
Saccade training („Gaze Jump Training“):
During saccade training, a single point is shown on the screen in front of the person concerned, which he or she should look at first (fixation point). At a beep, another dot or symbol appears that has to be discovered and to which the eyes are meant to jump (hence the term „saccades" = jumps). In this way, the brain is systematically trained to make more gaze jumps into the neglected half of the visual field.
Exploration Training:
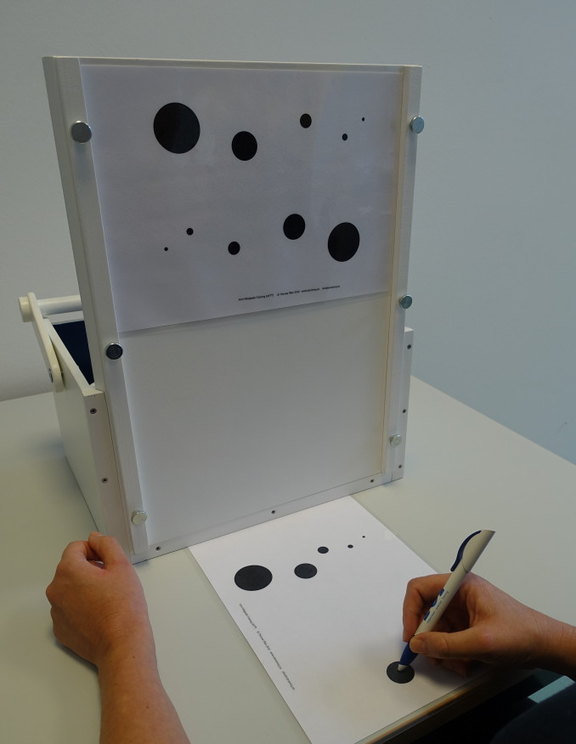
In daily life, we also need a visual overview. During exploration training, photos are asked to be scanned in their entirety and all of a certain category of objects should be discovered, e.g. all flowers of one color. In this way, the brain is trained to search the visual field more systematically and not to overlook relevant targets.
Neglect has a detrimental effect on our visual perception which can be improved by performing optokinetic stimulation, saccade training, and exploration training. Thereby, activity limitations in daily life caused by neglect can effectively be reduced.

Kerkhoff G und Schmidt L. Neglect und assoziierte Störungen. 2018. Hogrefe Verlag, Göttingen (ISBN 9783840928543).
Platz T, Winter T, Müller N, Pinkowski C, Eickhof C, Mauritz K-H. Arm Ability Training for Stroke and Traumatic Brain Injury Patients with mild arm paresis. A Single-Blind, Randomized, Controlled Trial. Archives of Physical Medicine and Rehabilitation 82: 961-968, 2001.
Platz T, Eickhof C, van Kaick S, Engel U, Pinkowski C, Kalok S, and Pause M.. Impairment-oriented training or Bobath therapy for arm paresis after stroke: a single blind, multi-centre randomized controlled trial. Clin Rehabil, 2005; 19:714-724
Platz T, van Kaick S, Mehrholz J, Leidner O, Eickhof C, Pohl M. Best conventional therapy versus modular Impairment-oriented training (IOT) for arm paresis after stroke: a single blind, multi-centre randomized controlled trial. Neurorehabilitation and Neural Repair 23:706-16, 2009.
Platz T und Lotze M. Arm Ability Training (AAT) Promotes Dexterity Recovery After a Stroke — a Review of Its Design, Clinical Effectiveness, and the Neurobiology of the Actions. Front. Neurol. 9:1082. doi: 10.3389/fneur.2018.01082
Thieme H, Morkisch N, Mehrholz J, Pohl M, Behrens J, Borgetto B, Dohle C. Mirror therapy for improving motor function after stroke. Cochrane Database Syst Rev. 2018 Jul 11;7(7):CD008449.